Death rates for mothers and newborn babies have increased for the first time in a decade amid growing concerns over patient safety, a report reveals.
There has been an ‘alarming decline’ in the overall quality of NHS care, with the deterioration in maternity services particularly bad, it adds.
Researchers at the Institute of Global Health Innovation in Imperial College London have noted a growing disparity between the UK and leading countries when it comes to mortality rates from preventable causes like sepsis and blood clots. According to their findings, this gap has become wider.
If the UK matched the top 10 per cent of OECD countries, this would save 13,495 people from dying each year.
The experts warn failings exposed in their 2024 National State of Patient Safety report must be addressed ‘urgently’.
Lord Darzi, who serves as one of the co-directors at the Institute of Global Health Innovation and recently headed a government-requested analysis of the NHS, expressed concern over the concerning trends identified in their most recent report on patient safety in England.
‘The deterioration in maternity care, in particular, requires immediate action.
‘Our analysis highlights a troubling increase in neonatal and maternal deaths, with black women disproportionately affected.’

A recent report has highlighted a troubling development: death rates among mothers and newborns have seen their first increase in ten years. This worrisome trend has raised significant worries regarding patient safety standards.

The experts warn failings exposed in their 2024 National State of Patient Safety report must be addressed ‘urgently’ (Stock image)
The report said its analysis of the most recent MBRRACE-UK reviews – an audit programme that collects data on the deaths of mothers and babies – and data from the Office for National Statistics ‘provides cause for concern’.
It found rates of neonatal deaths – babies born at 20 weeks or after, but who die before they are 28-days-old – and maternal deaths – women who die while pregnant or up to six weeks after due to issues linked to pregnancy – increased for the first time in ten years and are continuing to rise.
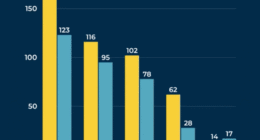
Between 2013 and 2020, the neonatal death rate fell by 17 per cent, from 1.7 to 1.3 per 1,000 live births.
But it rose to 1.5 per 1,000 live births in 2022, an increase of 15.4 per cent.
Maternal deaths were described as ‘steady’ between 2011 and 2013 and 2017 and 2019, although between 2017 and 2019 and 2020 to 2022, the rate increased from 8.8 to 13.4 deaths per 100,000.
The report described the figure as ‘a statistically significant increase of 52.3 per cent’.
The Care Quality Commission, the health standards watchdog, has previously warned maternity failings are so ‘widespread’ they risk becoming ‘normalised’, with two thirds of the services inspected in need of improvement or condemned as ‘inadequate’ for the safety of mothers and babies.
These issues come alongside growing concerns about access to urgent care and the ‘spiralling costs of unsafe care’, the Imperial College report said.

Maternal deaths were described as ‘steady’ between 2011 and 2013 and 2017 and 2019, although between 2017 and 2019 and 2020 to 2022, the rate increased from 8.8 to 13.4 deaths per 100,000
It added that ‘addressing patient safety in the NHS is not just a moral obligation but an urgent financial necessity’.
The estimated cost of treating patients who have been harmed during their care in England in 2023/24 was £14.7 billion.
This figure excludes wider costs, such as to people’s quality of life or their ability to work, or rising clinical negligence claims.
The report also highlights the uneven consequences of unsafe care, which are ‘greater in the North than the South’.
It found the unintended effects of medical treatment, meaning a resulting death or disability, are twice as high in the North East than in Greater London.
Members of the public, NHS staff and social care workers said waits for urgent care – including waiting to be seen in A&E or waiting for an ambulance – are their number one safety concern.
Rates of hospital-acquired Clostridium difficile have increased by 54 per cent between 2018/9 and 2023/24, raising concerns about the NHS slipping on progress tackling hospital infections in previous years.
Lord Darzi added: ‘The NHS is now falling behind leading nations in patient safety.
‘We urgently need to address these issues to repair the health service, and provide high-quality care for all patients and their families.’
Melanie Leis, a co-author of the report and director of policy and analysis at the Institute of Global Health Innovation, said: ‘Our analysis paints a worrying picture of patient safety across many areas, making it very difficult to choose specific areas to prioritise.’
James Titcombe, chief executive of the charity Patient Safety Watch, which commissioned the report, said its findings must ‘contribute to urgent and meaningful discussion’ about change to ensure trends are reversed when the data is revisited in 2026.
A Department of Health and Social Care spokesperson said: ‘Patient safety is paramount, and all women and their babies deserve safe, high-quality care.
‘We are working to introduce a culture of transparency in our health service and will never turn a blind eye to failure.
‘We are committed to driving up standards in healthcare through our Plan for Change, and we will tackle the shocking inequalities that exist across the country.
‘We will also work closely with NHS England to train thousands more midwives to better support women throughout their pregnancy and beyond.’